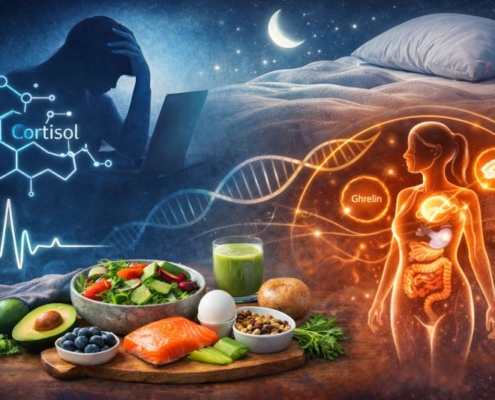
How Stress, Sleep and Hormones Affect Your Nutrition Needs
This matters because many people blame food choices or willpower, when the real drivers are disrupted stress hormones, poor sleep regulation or shifting hormonal demands. Addressing these factors alongside diet is often the missing step — and it’s where personalised nutrition support in London can help nutrition feel supportive rather than exhausting.
The short answer: hormones respond to lifestyle, not just food
Hormones act as messengers between the brain and body. They respond continuously to stress exposure, sleep patterns and energy availability. When these signals are disrupted, hunger cues, satiety, blood sugar regulation, digestion and recovery can all change — often without obvious warning.
Key drivers that shape nutrition needs include:
- Chronic psychological or physical stress
- Inconsistent or insufficient sleep
- Irregular eating patterns or under-fuelling
- Ongoing lifestyle pressure without adequate recovery
Supporting nutrition effectively often means understanding how these factors influence hormonal balance, rather than focusing on calories or macros alone, as explained in how nutrition can support hormones naturally.
How stress alters appetite, metabolism and food choices
Stress activates cortisol, a hormone designed to help the body cope with short-term challenges. When stress becomes ongoing, cortisol can remain elevated longer than intended, influencing blood sugar regulation, appetite timing and fat storage.
Common nutrition-related effects of chronic stress include:
- Reduced appetite earlier in the day
- Stronger cravings in the evening
- Digestive discomfort or bloating
- Greater reliance on caffeine or sugary foods
Over time, these patterns can affect where fat is stored, particularly around the abdomen, which is explored further in foods that support belly fat reduction.
Why sleep quality has a direct impact on hunger and energy
Sleep plays a key role in regulating hormones that control appetite and fullness. Even short periods of disrupted or insufficient sleep can increase hunger, reduce satiety and shift food preferences toward quick-energy options.
When sleep is poor, people often notice:
- Higher appetite the following day
- Reduced impulse control around food
- Lower energy for cooking or planning meals
- Less stable glucose regulation
This is why nutrition plans that ignore sleep often feel harder to follow long term, and why sleep is increasingly recognised as central to body composition and energy balance, as discussed in the link between sleep and weight regulation.
Hormonal fluctuations and changing nutrition needs
Hormonal needs are not static. Daily rhythms, life stages, stress exposure and recovery capacity all influence how the body responds to food. Appetite, digestion and energy requirements can shift even when eating habits remain unchanged.
During these transitions, targeted support can be helpful, which is why some people benefit from working with a nutritionist focused on hormone health when symptoms feel persistent or confusing.
The stress–sleep–nutrition feedback loop
Stress, sleep and nutrition influence one another continuously:
- Poor sleep increases stress sensitivity
- High stress disrupts hunger regulation
- Irregular eating patterns impair recovery and sleep quality
Breaking this cycle usually involves small, stabilising changes rather than strict or restrictive dietary overhauls.
What supportive nutrition looks like during high stress
When stress or poor sleep is present, nutrition strategies tend to focus on stability rather than optimisation.
Supportive approaches often include:
- Regular, balanced meals to stabilise blood sugar
- Adequate protein to support satiety and recovery
- Consistent eating patterns rather than prolonged fasting
- Simple structure that reduces decision fatigue
For some people, adding nourishment rather than removing foods — such as using simple, nutrient-dense options — can feel more supportive, as outlined in how collagen smoothies can support women during high-demand phases.
Why generic nutrition advice often falls short
One-size-fits-all advice rarely accounts for sleep debt, workload, emotional stress or recovery capacity. As a result, people may follow plans that look healthy on paper but feel exhausting or unsustainable in practice.
Personalised nutrition considers lifestyle pressures and hormonal responses alongside food choices — not instead of them.
When eating well feels harder than it should
If nutrition feels increasingly inconsistent, effortful or mentally draining, it may be a sign that stress and recovery need attention alongside food. Supporting these systems together often makes eating feel more intuitive and manageable again.
Frequently asked questions
Can stress affect nutrition even if I eat well?
Yes. Chronic stress alters cortisol levels, which can influence appetite, blood sugar regulation and digestion, even when food choices are balanced.
Why does poor sleep increase hunger?
Sleep disruption affects hormones that regulate hunger and fullness, often increasing appetite and reducing satiety the following day.
Do hormones influence weight and fat distribution?
Hormonal signals affect how energy is stored and used, including where fat is stored, particularly during periods of high stress or poor recovery.
Is it normal for nutrition needs to change over time?
Yes. Stress exposure, sleep quality and hormonal rhythms can change how the body responds to food, even if eating habits stay the same.
When should nutrition feel easier with support?
When stress, sleep and recovery are supported alongside food choices, nutrition often feels more sustainable and intuitive.
Long-term perspective
Nutrition does not exist in isolation. Stress exposure, sleep quality and hormonal rhythms shape how your body uses food every day. When these foundations are supported, nutrition becomes easier to maintain and more effective in supporting long-term wellbeing.